What is chronic pain?
Chronic pain is an unpleasant sense of discomfort that persists or progresses over a

long period. In contrast to acute pain that arises suddenly in response to a specific injury and is usually treatable, chronic pain persists over time and is often resistant to medical treatments.
We have previously discussed chronic pain caused by osteoarthritis. The following are scenarios that cause chronic pain of a non-osteoarthritic nature:
Maladaptive chronic pain
The treatment of the above conditions or scenarios is guided by the understanding of how the disease develops, progresses and behaves, in other words, its pathophysiology. In this article, let us focus on Maladaptive Chronic Pain.
What is Maladaptive Chronic Pain?
Maladaptive pain is termed as unnecessary pain. This is because the pain caused by damaged tissues persists long after healing has occurred so that the pain becomes the problem, rather than the tissues from which the pain comes [2]. Maladaptive pain is protracted in duration, exaggerated in severity, and expanded in the field, and can occur in the absence of obvious tissue pathology. The types of disease conditions causing these pain syndromes are many and poorly understood [3]. They include:-
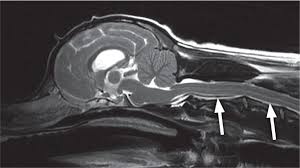
1. Central nervous system lesions, including post-trauma or vascular accidents, intracranial masses, and congenital defects (e.g., syringomyelia)
2. Chronic intervertebral disk disease
3. Diabetic neuropathy
4. Feline hyperesthesia syndrome
5. Feline orofacial pain syndrome
6. Postperipheral nerve injury (e.g., trauma, amputation)
7. Postsurgical conditions (e.g., fractures, hernia repair)
8. Others
We have previously discussed the signs and symptoms of chronic pain here.
Management Of Maladaptive Pain
Maladaptive pain is managed by combining both non-steroidal anti-inflammatory drugs (NSAIDs) and opioids. NSAIDs are usually the first-line drugs, but because of the progressive nature of maladaptive pains, a multimodal approach therapy that includes NSAIDs, opioids and neuromodulatory agents, is usually used.
1. NSAIDs
Table 1: Non-Steroidal Anti-Inflammatory Agents (NSAIDs)
Selected NSAIDs Data for Dogs and Cats Drug Species Route Dose (mg/kg)
Aspirin Dog Intravenous 44mg/kg Cat Oral 2.5mg/kg
Carprofen Dog Oral 2mg/kg Subcutaneously 2mg/kg Cat Intravenous 4mg/kg
Celexocib Dog Intravenous 5mg/kg
Deracoxib Dog Oral 1-5mg/kg Cat Oral 1mg/kg
Etodolac Dog Oral 10-15mg/kg
Firocoxib Dog Oral 5mg/kg
Ketoprofen Dog Intravenously, 2mg/kg once, then orally 1mg/kg
Intramuscularly, daily
Subcutaneously Cat Oral 1mg/kg
Meloxicam Dog Oral 0.2mg/kg Oral 0.1mg/kg
Piroxicam Dog Oral 0.3mg/kg Cat Oral 0.3mg/kg
Robenacoxib Cat Subcutaneously 2mg/kg Dog Subcutaneously 2mg/kg
Tepoxalin Dog Oral 10 - 20mg/kg
This site provides a useful calculator to convert laboratory values, dosages, and other measurements to SI units
2. Neuromodulatory agents
Table 2: Neuromodulatory agents
Neuromodulatory agents Drug Species Route Dose (mg/kg)
Gabapentin Dog/Cat Oral 10-30mg/kg
Pregabalin Dog Oral 3-4mg/kg Cat Oral 1-2mg/kg
Amitriptylin Dog Oral 1-2mg/kg Cat Oral 0.5-1mg/kg
Tramadol Dog Oral 5mg/kg
Amantadine Dog Oral 3-5mg/kg
Acetaminophen + hydrocodone Dog Oral 10 mg/kg
Intravenous Constant Release Dog Intravenous 0.25-0.5 mg/kg
Infusion of ketamine
Intravenous Constant Release Dog Intravenous 1mg/kg
Infusion of lidocaine
This site provides a useful calculator to convert laboratory values, dosages, and other measurements to SI units
3. Weight optimization
Obesity is a risk factor for both the incidence and progression of osteoarthritis, maladaptive pain, and it has a negative influence on outcomes. Loss of at least 10% of body weight, coupled with exercise, is recognized as a cornerstone in the management of obese patients with osteoarthritis and maladaptive pain and can lead to significant improvement in symptoms, pain relief, physical function and health-related quality of life.
4. Physical modalities
Acupuncture
Myofascial trigger point therapy
Physical therapy (therapeutic exercises, hydrotherapy)
Energy-based modalities (therapeutic laser, extracorporeal shock wave therapy)
Further reading
References
[1] L. Ray, R. B. Lipton, M. E. Zimmerman, M. J. Katz and C. A. Derby, "Mechanisms of association between obesity and chronic pain in the elderly," PAIN®, vol. 152, no. 1, pp. 53-59., 2011.
[2] K. A. Mathews, "Neuropathic pain in dogs and cats: if only they could tell us if they hurt," Veterinary Clinics of North America: Small Animal Practice, vol. 38, no. 6, pp. 1365-1414, 2008.
[3] K. A. Kirkby and D. D. Lewis, "Canine hip dysplasia: reviewing the evidence for nonsurgical management.," Veterinary Surgery, vol. 41, no. 1, 2012.
[4] R. I. Krontveit, C. Trangerud, B. K. Sævik, H. K. Skogmo and A. Nødtvedt, "Risk factors for hip-related clinical signs in a prospective cohort study of four large dog breeds in Norway.," Preventive veterinary medicine, vol. 103, no. 2-3, pp. 219-227., 2012.
[5] B. KuKanich and M. G. .. Papich, "Pharmacokinetics and antinociceptive effects of oral tramadol hydrochloride administration in Greyhounds.," American Journal of veterinary research, vol. 72, no. 2, pp. 256-262, 2011.
[6] Mypet.com, "About diabetes mellitus," Mypet.com, [Online]. Available: https://www.mypet.com/pet-diabetes/dogs-cats.aspx. [Accessed 17 October 2020].
[7] M. E. Goldberg, "A look at chronic pain in dogs," Veterinary Nursing Journal,, vol. 32, no. 2, pp. 37-44, 2017.
[8] C. A. T. Buffington, " Idiopathic cystitis in domestic cats—beyond the lower urinary tract.," Journal of Veterinary Internal Medicine, vol. 25, no. 4, pp. 784-796, 2011.
[9] M. Kent, Oxford Dictionary of Sports Science and Medicine. Reference Reviews., 3rd ed., Oxford University Press, 2006.
[10] C. J. Woolf, "Pain: moving from symptom control toward mechanism-specific pharmacologic management.," Annals of internal medicine, vol. 140, no. 6, pp. 441 - 451, 2004.
[11] D. M. Boothe, "NSAIDs: It is Not Just About the Pain," 2019.
[12] Rusbridge C, Heath S, Gunn-Moore D A, Knowler S P, Johnston N, McFadyen A K (2010) Feline orofacial pain syndrome (FOPS): a retrospective study of 113 cases.J Feline Med Surg12(6), 498-508
[13] Marbach J J (1999) Medically unexplained chronic orofacial pain. Temporomandibular pain and dysfunction syndrome, orofacial phantom pain, burning mouth syndrome and trigeminal neuralgia. The Medical Clinics of North America 83 (3), 691-710 PubMed.






















Comments